Downstream Transportation Impacts of Medicaid Cuts & Changes
Situational Awareness from the Regional Alliance for Resilient and Equitable Transportation (RARET)

This blog was produced by the Regional Alliance for Resilient and Equitable Transportation (RARET), a coalition of Hopelink Mobility Management focused on transportation problem solving surrounding emergency events in King, Pierce, and Snohomish counties with a focus on access and functional needs. Reach out to Dean Sydnor (DSydnor@hopelink.org) to learn more about RARET.
The current Congressional Budget Office assessment of pending legislation outlines significant reductions in the number of Medicaid recipients, with a trillion dollars in cuts and millions projected to lose coverage. Governor Bob Ferguson’s office declared this “will fundamentally alter Washington’s health care system and result in hundreds of thousands of Washingtonians losing their health care”.
What is Medicaid?
Medicaid is a means-tested program that finances primary and acute medical services as well as long-term services and supports. A means-tested program is one that assesses eligibility based on income. Medicaid is jointly funded by the federal government and the states. The federal government's share of most Medicaid expenditures is called the Federal Medical Assistance Percentage (FMAP). The remainder is referred to as the state share.
Roughly 1 in 5 Washingtonians (approx. 2 million people) rely on Apple Health, WA’s Medicaid program, for their healthcare coverage. At least 250,000 Washingtonians are estimated to lose coverage over the next ten years. The impacts of this federal legislation are wide-ranging, and its effect on the transportation landscape of the central Puget Sound and beyond should not be overlooked. See the HCA’s fact sheet breaking down the impacts to Washington State for more details.
Immediate impacts: Coverage Losses & NEMT
Non-emergency Medical Transportation (NEMT) in Washington is a transportation system that connects people to transportation resources, facilitating access to their Medicaid-billable appointments. It does this in a few ways; Medicaid recipients with transportation benefits are either lower-mode or higher-mode clients of NEMT. Lower-mode clients can take fixed route transit and receive bus-fare and/or gas-reimbursement for their medical trips. Higher-mode clients’ doctors provide a note to the NEMT brokerage explaining the medical reason they cannot take fixed-route transit, which justifies the NEMT broker arranging door-to-door transportation for these clients via one of their contracted transportation service providers. A big advantage of NEMT is that it has complete coverage over an entire region, whereas services like ADA Paratransit can only mirror fixed-route service areas in a region, which can create gaps in rural areas where fixed-route services are scarce. In short, NEMT facilitates rides, bus fare, and gas reimbursement to get people to and from Medicaid billable healthcare.
- NEMT is funded by Medicaid packages with transportation benefits providing services like door-to-door rides, bus fare, and gas reimbursement.
- NEMT in Washington uses brokerages that take calls and arrange trips for contracted transportation providers paid by Medicaid.
- The brokers in the Central Puget Sound region are Hopelink NEMT (King/Snohomish) and Paratransit Services (Pierce).
The good news is that NEMT is legally protected and cannot be altered without specific legislation. But that good news won’t help clients who lose Medicaid coverage. If an individual's coverage lapses or is terminated, NEMT services cannot be provided. The immediate impact will fall on patients and healthcare facilities attempting to coordinate transportation - particularly for discharges. For instance, discharging a Medicaid patient from the ER typically involves a simple call to the NEMT broker to arrange transport. Without active Medicaid coverage, that option disappears. As a result, patients with limited financial means and already overburdened hospitals will be left to manage transportation on their own, placing additional strain on both vulnerable individuals and the healthcare infrastructure.
As noted above, lower-mode clients often rely on free bus rides, including transfers, to travel to and from medical appointments and to connect with other essential services. These connections are critical in preventing patients from quickly returning to the healthcare facility. Without access to Non-Emergency Medical Transportation (NEMT), these low-cost transportation options may no longer be available, making it more difficult for patients to reach care facilities and related services unless an alternative, affordable transit option is provided.
- An immediate transportation impact of Medicaid cuts is that healthcare facilities lose the ability to leverage a vital service to get those formerly-Medicaid covered patients back home.
Medium-to-Long Term Impacts
Over the long term, this issue will escalate as clients who lose coverage may skip preventive care and rely solely on emergency rooms for treatment. This will increase demand for emergency room services, while simultaneously reducing the resources available to help patients return home after receiving care. While NEMT does not transport to emergency rooms, many NEMT trips are conducted to urgent care facilities. If Medicaid stops covering appointments, and therefore the associated transportation, some people may be forced to use an ambulance and go to the ER for issues that previously would have been addressed at a standard medical appointment. These cuts could reduce staffing levels or even cause some healthcare facilities, especially in rural areas, to close. This affects transportation for both those who lose coverage and those who don’t. With fewer staff, patients may face longer wait-times for return rides, especially later in the day when transportation services are limited. If rural facilities close, trips become longer and more expensive for those who are not NEMT clients. Even those who still have NEMT may face problems if brokers don't have enough drivers to handle the longer rural-to-urban trips. Transportation providers may also shrink in number, since their income depends on the volume of clients they transport. Fewer clients results in less funding to sustain their operations.
Summary:
- Higher ER demand with fewer transportation solutions
- Longer travel times and wait times
- Less resources for NEMT transportation service providers
Beyond Hospitals: At Home Care and Nursing Homes
Another concern involves those receiving Medicaid covered at-home services. The risk for these people is two-fold: they may lose coverage entirely, but even if they do not, the reduced program funding may render certain at-home services financially unsustainable. Typically, these at-home services are being used precisely because travelling is impractical or even impossible. If they must now travel for those same services, clients must now find their own transportation where they had not before, even if they still have coverage. There is the danger too that these services may no longer be covered at all, whether at home or at a facility, in which case the clients may find themselves using more emergency services down the line.
Medicaid supports 3 in 5 Washingtonian nursing home residents. The downstream transportation impacts are significant, regardless of what alternative solutions are implemented. Clients living in Skilled Nursing Facilities (SNFs) are often extremely difficult to transport safely without compromising their health and well-being. While NEMT can be a suitable option for some residents, losing access to it may force the use of more specialized, and more expensive, transportation services. These clients are likely not compatible with a shift to modes of transportation other than door-to-door service. In some cases, emergency services may have to be used unnecessarily, despite NEMT being the more appropriate and cost-effective choice that they would have formerly qualified for.
Solutions
Mobility Management frameworks reduce mobility challenges, but in situations like this, a transportation option is being removed without an equivalent replacement. Individuals and their assistors need support to understand how their benefits will be impacted. A critical concern is thatpeople, who would otherwise be covered, lose their coverage due to lapses in paperwork or other administrative issues; this would still result in NEMT being unable to facilitate rides. The reason for the lapse in coverage does not determine whether NEMT can provide transportation services. Avoiding preventable reasons for a coverage lapse should be a critical concern.
- There is not an easy 1:1 replacement for not being able to move folks with NEMT. If a coverage loss or lapse can be prevented, creating a plan for maintaining coverage is critical to ensuring continued access to NEMT.
The immediate option that many folks may seek out will be ADA Paratransit services. Their door-to-door services for those who cannot take the bus makes them a logical place for those who would be former higher-mode clients of NEMT. ADA Paratransit has a different eligibility process than NEMT higher-mode; there is no guarantee they will qualify for ADA Paratransit. If a client is fortunate enough to qualify for Paratransit, it can take up to 21 days after a completed application submittal to secure their first ride.
- ADA Paratransit is an option people will turn to. ADA eligibility is a unique process that takes time, and their operations may not have the resources for a rapid increase in demand.
If a client cannot use NEMT and has not yet completed the ADA paratransit assessment, their transportation options diminish. While some local services may offer alternatives, same-day transportation is rarely available. Some clients will look at private pay/out-of-pocket solutions to transportation challenges. However, these options, especially for wheelchair accessible cabulances, can be too costly, especially for clients who were formerly beneficiaries of means-tested programs like Medicaid. As a result, more clients may have to rely on fixed-route buses due to their lower cost per ride and no per-mile charge for clients. This marks a significant change in how people will get around, especially for those used to door-to-door NEMT service. This transition, known as a mode shift in mobility management, can be challenging.
Support Our Communities
- Helping clients access reduced fare programs such as ORCA LIFT, the Subsidized Annual Pass, and the Human Service Bus Ticket program can help reduce financial strain on both the clients and the facility.
- To ease mode shift changes, facilities should work with local transit agencies to obtain educational materials like route maps and provide training for staff on how to assist clients.
- While coverage is not universal, some alternatives exist locally that could mitigate the impact of this change. Services like the Sound Generations Hyde Shuttle, Beyond the Borders, and Homage’s Transportation Assistance Program are all examples of services that could offer vital connections for clients. Using service discovery tools can be helpful in determining if clients would be a good fit for these local solutions.
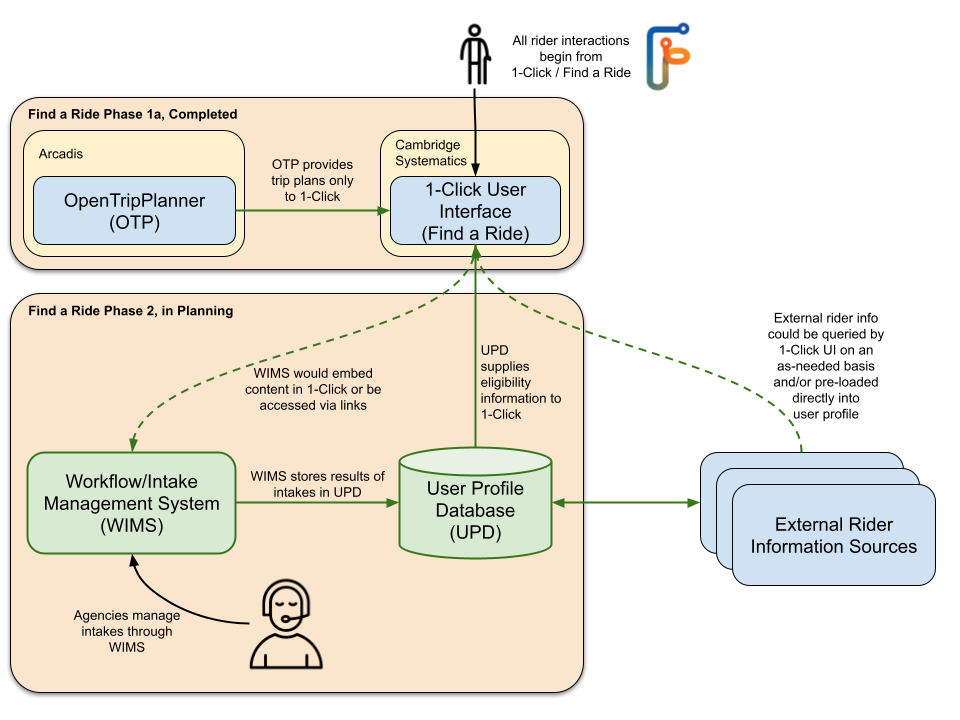
- FindARide.org includes a service directory and trip planner for targeted and efficient travel planning. For those in Snohomish, King, and Pierce counties, FindARide.org offers a trip planner and list of resources that captures transportation solutions that include local options like volunteer driver programs, services for seniors, demand response vehicles for people who use wheelchairs, or who have other access needs, and more. If you are not sure what services exist, it is a great place to start. If you would like to connect with Find a Ride’s team about training opportunities, please reach out to FindARide@hopelink.org.
- More folks will have to take fixed-route buses or delay care altogether.
Ongoing Situational Awareness
To keep up to date on transportation developments in the region, connect with King County Mobility Coalition (KCMC), the Snohomish County Transportation Coalition (Snotrac), or Pierce County Coordinated Transportation Coalition (PCCTC), depending on your geography. The KCMC hosts regular Access to Health and Wellbeing (AtHW) Workgroup meetings, which are regionally relevant and can be a good venue to discuss transportation barriers in healthcare with knowledgeable parties.
RARET will continue to monitor situational awareness on this subject. If you have information to share about transportation impacts of changes to Medicaid, reach out to Dean Sydnor, RARET Program Supervisor, at DSydnor@hopelink.org.
Mobility News